Next Generation & the Future of Erectile Dysfunction Treatments
Erectile dysfunction also synonymously known as ED affects nearly half of men between the ages of 40 and 70 to some extent. Vascular diseases interrelated with aging, hyperlipidemia, smoking, diabetes as well as hypertension, are often linked to erectile dysfunction. Furthermore, injury to cavernous nerves in the penile region “comprises an appreciable number of ED cases.” 6 Other causes of erectile dysfunction include but are not limited to endocrine disorders, as well as fibrosis of the penile tissue and corporal smooth muscle.11 Overall both vasculogenic and neurogenic erectile dysfunctions are linked to the loss of normal cellular function or cell death (apoptosis).
Oral medications such as phosphodiesterase-5 inhibitors (PDE5is), have clear benefits, and are typically first-line treatments in regards to erectile dysfunction, however their actions are short lived.6 Lifestyle changes and injections are also typical first line treatment options for the management of complex cases of erectile dysfunction. Most recently scientists and physicians have been focusing on new next generation novel therapy options as a way to restore natural sexual function; one such treatment option includes Stem Cell based Bioactive Factor Therapy.
Stem-cell-based therapies focus on the management of erectile dysfunction “through the protection of the threatened host cells via immunomodulatory effects, and the provision of trophic factors or gene delivery.”11 In recent years, a number of research studies related to the progress of stem cell-based erectile dysfunction therapy have been published. This is yielding strong evidence supporting the concept that stem-cell-based bio-active therapy is potentially the next generation therapeutic approach for erectile dysfunction. Furthermore, research studies conducted have taken into account a large spectrum of stem cells, including mesenchymal stem cells, tissue as well as muscle -derived stem cells for further investigation in regards to vascular, neural, endothelial or smooth muscle regeneration in animal models for erectile dysfunction.
What are Mesenchymal Stem Cells?
Stem cells are cells that differentiate into smooth muscle cells, neurons, endothelial cells and other types of varying cells. Stem cells by definition have the capability of self-renewal, meaning that they can make copies of themselves for an indefinite period, and differentiate into a variety of phenotypes.1, 2 Stem cells are defined by their “capacity for both self-renewal and directed differentiation. Thus, they represent great promise for regenerative medicine.” Stem cells can be categorized as either embryonic stem cells (ESCs) or adult stem cells (ASCs). Embryonic stem cells (ESCs) are acknowledged as an example of pluripotent cells.6 While multipotent stem cells include mesenchymal stem cells (MSCs) as they “are capable of self-renewal, and they can differentiate into any cell type within their germ layer”.4
Stem cells have diverse properties that make them potentially viable for utilization in various disease treatments. In particular, adult MSCs are “multipotent cells that undergo self-renewal and differentiation” as well as express specific surface markers.13 MSCs can be derived from different sources within the body, including adipose tissue, bone marrow as well as the umbilical cord membrane. 13, 12 Historically, MSCs were founded by a researcher named Friedenstein through the conduction of studies on the bone marrow although MSCs can be isolated from other adult tissues including adipose tissue. 7, 5 The word “Stem Cells” more correctly known as “Mesenchymal Stem Cells” (MSCs) were termed MSCs secondary to their innate ability to duplicate while maintaining the attribute of multi-potential lineage.
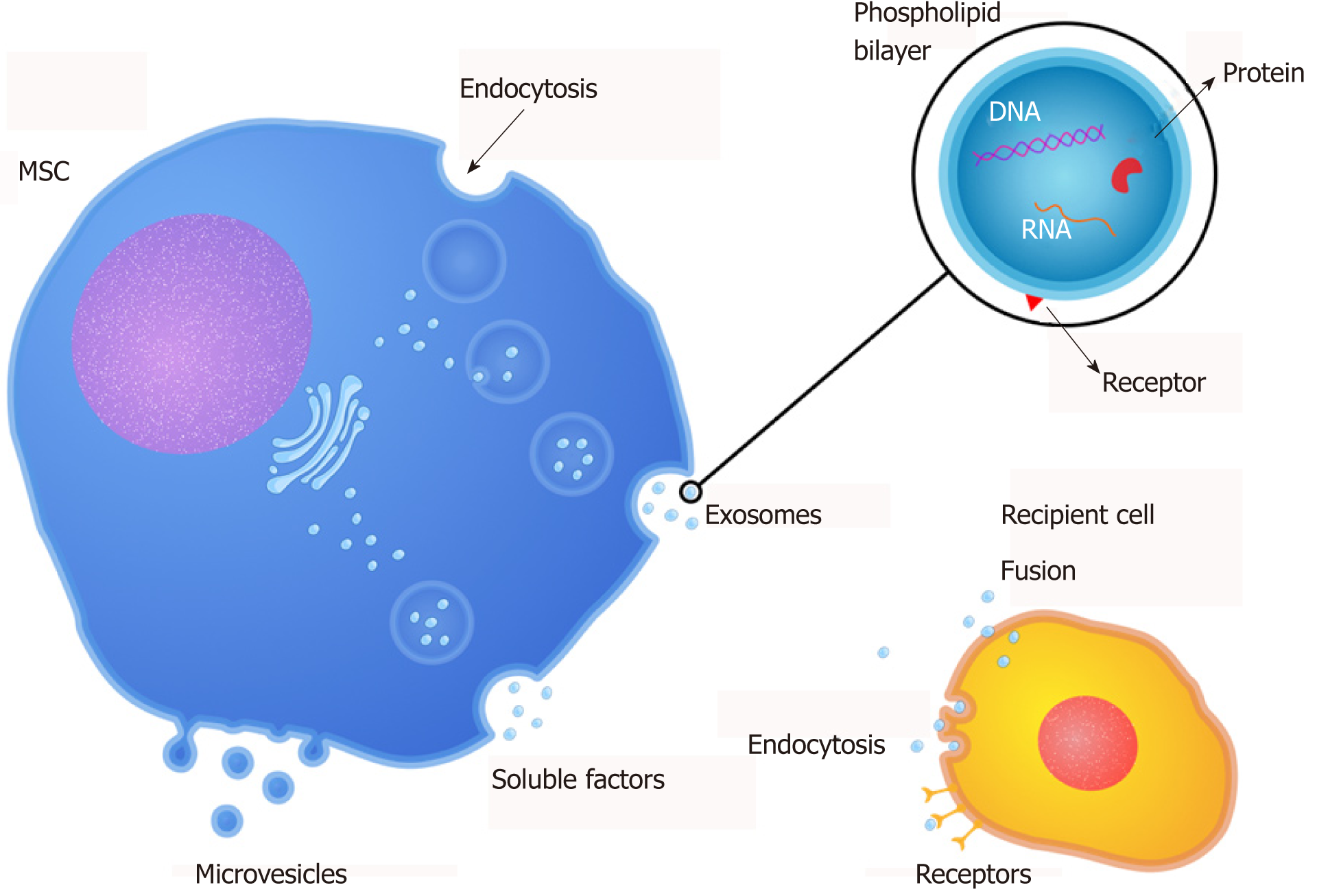
MSCs “contain growth factors, signaling lipids, mRNAs, and regulatory miRNAs, which are involved in tissue repair as paracrine mediators.” 13, 14 Research studies have also suggested that exosomes released by MSCs may aid erectile dysfunction linked to diabetes through anti-fibrotic mechanisms, preventing cell death as well as increasing smooth and endothelial muscle content. 15, 18
What are Bioactive Factors and EVs?
MSCs are able to secrete soluble “Bioactive Factors” which aid in modulating the immune system, improve the standard rate of healing injured tissues and reduce inflammation. Stem Cell Bioactive Factors consist of nanoparticles which are released from the membranes of Mesenchymal Stem Cells (MSCs). These nanoparticles contain over “200 Growth factors, Cytokines and Nucleic Acids which support healthy cell-to-cell communication and are responsible for the therapeutic effects observed in regenerative medicine.”
EVs or extracellular vesicles are membrane-packed vesicles that are secreted by MSCs. 9 EVs have been demonstrated to perform a critical role in cell-to-cell communication and important processes such as immune responses, homeostasis maintenance, and more. 8, 9
Microvesicles, an important EV, may “change functional target cells by delivering intracellular proteins”; for example, MVs released from endothelial cells can promote the regeneration through transfer of growth factors and their activators. 12 MSC-derived EVs (MSC-EVs) based stem cell therapies are easier to manage and safer “due to their inability to directly form tumors.” 10
Mesenchymal Stem Cell’s Bioactive Factors
Bioactive Factors demonstrate numerous advantages when compared to Mesenchymal Stem Cells:
Essentially Bioactive Factors exert far more therapeutic effects than Mesenchymal Stem Cells could.
Therapeutic Effects of Stem Cell Bioactive Factors

Growth factors, Cytokines and Nucleic Acids within Stem Cell Bioactive Factors are catalysts for regeneration as they contribute to tissue and organ repair, alter inflammation, aid in neural communication, improve mitochondrial viability and participate in the alteration of aging cells. Overall Bioactive Factors derived from Stem Cells aid the body in repairing damaged tissues and injuries.
Stem Cell Bioactive Factors have been utilized by Medical Professionals for a number varying aspects including but not limited to soft tissue repair, and restoring sexual wellness. In regards to men’s sexual health Stem Cell Therapy rejuvenates, repairs and regenerates damaged penile tissues, aiding in the restoration of erectile function which may contribute to the elimination the need for long term reliance on drugs.
Some Examples of Bioactive Factors
How Boston Medical Group Sources Bioactive Factors

Boston Medical Group utilizes Bioactive Factors produced from an FDA-registered Tissue Banks which follow strict GMP guidelines as well as implement and maintain FDA regulations. The Tissue Bank sources from the highest quality donors and harvests from the healthiest part of the placenta in order to produce viable MSCs from which secreted Bioactive Factors are collected at the highest point potency. Upon the completion of manufacturing, each batch is sent for third party testing regarding microbiology and other safety protocols.
Clinic Trials Regarding Stem Cell Therapies and Erectile Dysfunction

Stem Cell Therapy can utilize varying types of stem cells including MSCs. Stem cells may also treat erectile dysfunction by supporting penile tissue through paracrine or hormone effects such as the “release of repair cytokines triggering endogenous mechanisms of regeneration separate from the trans-differentiation of stem cells into different cell types.” 14 Furthermore MSCs do not necessarily need to be engrafted within tissue to create a functional and structural response to the therapy administered.
Phase one studies in humans have shown “results in terms of tolerability, safety, and efficacy of use of stem cell transplant for the treatment of erectile dysfunction.” 18 Recent studies have also suggested that the combination Shock Wave Therapy and Stem Cell Therapy may decrease cell destruction within the penile corpora region as well as promote the growth of new blood vessels. 19
A literature review from ScienceDirect regarding the efficacy of Stem Cell Therapy revealed that five previously completed human clinical trials did show promise for Stem Cell Therapy as “being a restorative treatment option for erectile dysfunction”.20 The five studies included in the literature review utilized different types of stem cells, including various mesenchymal stem cells (MSCs). A total of 61 patients were included in the give studies, with mean ages of men being between 50 and 70 years. The literature review found that the majority of the five studies suggested improvement in erectile function and vascular flow in the penile region due to stem cell therapy without the report of serious adverse events occurring during the follow-up period. 20
Stem Cell Therapy may be a paradigm shift in the growing number of treatment options available for erectile dysfunction. Stem Cell Therapy has been recognized for its therapeutic properties in regards to aiding in treatment for various conditions including erectile dysfunction. Boston NextGen
Therapy embraces the latest in advanced technologies to help men restore erectile function without the use of drugs or the long term reliance on drugs. Boston Medical Group utilizes treatment protocols which are personalized to the individual’s conditions and may combine regimens such as shockwave therapy called RejuvaPulse
Therapy, BostonPRP
Injections and Stem-Cell Bioactive Factors. Thanks to a vast amount continuing research and development, Boston Medical Group physicians have culminated the most efficacious treatment protocols and continue to be the market leader in the field Erectile Dysfunction.
Boston Medical Group’s Optimum Regenerative Solution

Boston Medical Group utilizes the latest in next generation revolutionary treatment options for Erectile Dysfunction while upholding to GMP guidelines, and the utmost standards or requirements regarding the utilization of FDA registered tissue procurement organizations for Stem Cell Therapy. Boston Medical Group utilizes Bioactive Factors and EVs secreted from the membranes of placental-derived MSCs (Mesenchymal Stem Cells) which possess more than 200 growth factors as well as other immune factors which can render considerable therapeutic benefits, especially in the field of Regenerative Medicine***.
References
Figure 1. https://www.wjgnet.com/1948-0210/full/v11/i9/618.htm#F1
via Boston Medical Group https://ift.tt/2Ui5Qin
March 18th, 2020
